Quick-acting targeted therapies with minimal side effects are an urgent need for the treatment of anxiety-related disorders. While delta opioid receptor (DOP) agonists have shown ‘anxiolytic’ or anxiety-reducing effects, their mechanism of action is not well-understood. A new study by researchers from Tokyo University of Science highlights the role of specific neuronal circuits in the brain involved in the development of anxiety, and distinct mechanisms of action of the therapeutic DOP agonist – KNT-127.
Anxiety-related disorders can have a profound impact on the mental health and quality of life of affected individuals. Understanding the neural circuits and molecular mechanisms that trigger anxiety can aid in the development of effective targeted pharmacological treatments. Delta opioid receptors (DOP), which localize in the regions of the brain associated with emotional regulation, play a key role in the development of anxiety. Several studies have demonstrated the therapeutic effects of DOP agonists (synthetic compounds which selectively bind to DOPs and mimic the effect of the natural binding compound) in a wide range of behavioral disorders. One such selective DOP agonist—KNT-127—has been shown to exert ‘anxiolytic’ or anxiety-reducing effects in animal models, with minimal side effects. However, its mechanism of action is not clearly understood, thereby limiting its widespread clinical application.
To bridge this gap, Professor Akiyoshi Saitoh, along with Ms. Ayako Kawaminami and team from the
Tokyo University of Science, Japan, conducted a series of experiments and behavioral studies in mice. Explaining the rationale behind their work, Prof. Saitoh says, “There are currently no therapeutic drugs mediated by delta opioid receptors (DOPs). DOPs likely exert anti-depressant and anti-anxiety effects through a mechanism of action different from that of existing psychotropic drugs. DOP agonists may, therefore, be useful for treatment-resistant and intractable mental illnesses which do not respond to existing treatments.” Their study was published on 29 December 2024, in Neuropsychopharmacology Reports,
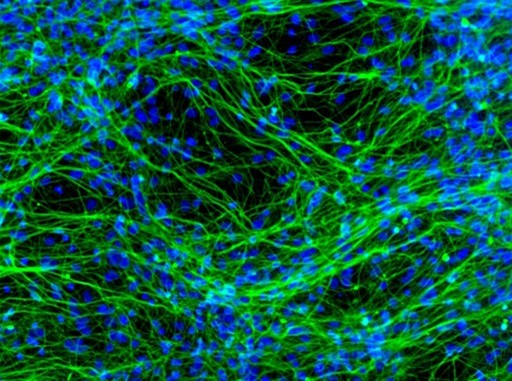
The neuronal network projecting from the ‘prelimbic cortex’ (PL) of the brain to the ‘basolateral nucleus of the amygdala’ (BLA) region, has been implicated in the development of depression and anxiety-like symptoms. The research team has previously shown that KNT-127 inhibits the release of glutamate (a key neurotransmitter) in the PL region. Based on this, they hypothesized that DOP activation by KNT-127 suppresses glutamatergic transmission and attenuates PL-BLA-mediated anxiety-like behavior. To test this hypothesis, they developed an ‘optogenetic’ mouse model wherein they implanted a light-responsive chip in the PL-BLA region of mice and activated the neural circuit using light stimulation. Further, they went on to assess the role of PL-BLA activation on innate and conditioned anxiety-like behavior.
They used the elevated-plus maze (EPM) test, which consists of two open arms and two closed arms on opposite sides of a central open field, to assess behavioral anxiety in the mice. Notably, mice with PL-BLA activation spent lesser time in the central region and open arms of the maze, compared to controls, which was consistent with innate anxiety-like behavior. Next, the researchers assessed conditioned fear response of the animals by exposing them to foot shocks and placing them in the same shock chamber the following day without re-exposing them to current. They recorded the freezing response of the animals which reflects fear. Notably, animals with PL-BLA activation and controls exhibited similar behavior, suggesting that distinct neural pathways control innate anxiety-like behavior and conditioned fear response.
Finally, they examined the effects or KNT-127 treatment on anxiety-like behavior of mice using the EPM test. Remarkably, animals treated with KNT-127 exhibited an increase in the percentage time spent in the open arms and central field of the maze, compared to controls. These findings suggest that KNT-27 reduces anxiety-like behavior induced by the specific activation of the PL-BLA pathway.
Overall, the study reveals the role of the PL-BLA neuronal axis in the regulation of innate anxiety, and its potential function in DOP-mediated anxiolytic effects. Further studies are needed to understand the precise underlying molecular and neuronal mechanisms, for the development of novel therapies targeting DOP in the PL-BLA pathway.
Highlighting the long-term clinical applications of their work, Prof. Saitoh remarks, “The brain neural circuits focused on in this study are conserved in humans, and research on human brain imaging has revealed that the PL-BLA region is overactive in patients with depression and anxiety disorders. We are optimistic that suppressing overactivity in this brain region using DOP-targeted therapies can exert significant anxiolytic effects in humans.”